IBS: A hidden epidemic that affects millions
What is Irritable Bowel Syndrome?

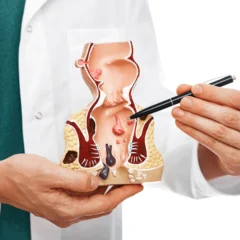
Irritable bowel syndrome (IBS) is a common disorder that affects the large intestine, causing symptoms such as abdominal pain, cramping, bloating, gas, diarrhoea, or constipation. IBS is not a disease, but a functional disorder, which means that there is no structural damage or inflammation in the intestine, but the way it works is abnormal.
IBS affects about 10% to 15% of the population worldwide, and it is more common in women than men. IBS can affect your quality of life and cause emotional distress, but it does not lead to serious complications or increase your risk of colon cancer
What Causes IBS?

The exact cause of IBS is not known, but several factors may play a role in triggering or worsening the symptoms. These include:
Muscle contractions in the intestine. The intestine has layers of muscle that contract and relax to move food and waste through the digestive tract. If these contractions are too strong or too weak, they can cause pain, gas, or changes in bowel habits.
Nervous system problems. The intestine has a network of nerves that communicate with the brain and control the digestive process. If these nerves are overactive or under active, they can make the intestine too sensitive or too slow, resulting in discomfort or altered bowel movements.
Inflammation in the intestine. Some people with IBS may have low-grade inflammation in the lining of the intestine, which can affect the normal function of the gut and cause pain or diarrhoea.
Infection or imbalance in gut bacteria. Sometimes, IBS can develop after a bout of gastroenteritis (stomach flu) caused by bacteria or viruses. This may alter the balance of good and bad bacteria in the gut, which can affect digestion and immunity. Some people with IBS may also have an overgrowth of bacteria in the small intestine, which can produce excess gas and bloating2.
Food intolerance or sensitivity. Certain foods may trigger or worsen IBS symptoms in some people. These include foods that are high in fat, spicy, dairy, gluten, fructose, or FODMAPs (fermentable oligo-, di-, mono-saccharides and polyols). FODMAPs are carbohydrates that are poorly absorbed in the small intestine and can cause gas and diarrhoea when fermented by bacteria in the large intestine.
Stress or psychological factors. Stress can affect the nervous system and the gut-brain axis, which is the communication between the brain and the digestive system. Stress can make the intestine more sensitive and reactive, causing pain or changes in bowel habits. Psychological factors such as anxiety, depression, trauma, or abuse can also influence IBS symptoms or make them worse.
How is IBS Diagnosed?
There is no specific test to diagnose IBS. The diagnosis is based on your medical history, physical examination, and ruling out other possible causes of your symptoms. Your doctor may ask you about your symptoms, their frequency and severity, how they affect your daily life, and any factors that trigger or relieve them. Your doctor may also perform some tests to exclude other conditions that can mimic IBS, such as:
Blood tests. To check for anaemia, inflammation, infection, or celiac disease.
Stool tests. To check for blood, parasites, bacteria, or inflammation markers.
Breath tests. To check for lactose intolerance or bacterial overgrowth in the small intestine.
X-rays or CT scans. To look for structural abnormalities in the abdomen.
Endoscopy. To examine the inside of the oesophagus, stomach, and small intestine with a thin tube and a camera.
Colonoscopy. To examine the inside of the colon and rectum with a thin tube and a camera.
How is IBS Treated?
There is no cure for IBS, but there are ways to manage the symptoms and improve your quality of life. It may include dietary changes, medications, probiotics, psychological therapies, or alternative therapies. You may need to try different options to find what works best for you. Some general tips are:

Dietary changes. You may need to identify and avoid foods that trigger or worsen your symptoms. You may also benefit from eating smaller and more frequent meals, drinking enough fluids, and increasing your intake of fibre-rich foods such as fruits, vegetables, whole grains, nuts, and seeds. However, some people with IBS may have difficulty tolerating certain types of fibre, such as those found in wheat, rye, barley, beans, lentils, and some fruits and vegetables. These are called FODMAPs (fermentable oligo-, di-, mono-saccharides and polyols), and they can cause gas and diarrhoea when fermented by bacteria in the large intestine. You may want to try a low-FODMAP diet, which involves eliminating these foods for a few weeks and then reintroducing them one by one to see how they affect you. A low-FODMAP diet should be done under the guidance of a dietitian or a GI doctor .
Medications. There are various medications that can help with different aspects of IBS symptoms, such as pain, spasms, diarrhoea, or constipation. These include antispasmodics, antidiarrheals, laxatives, fibre supplements, antidepressants, antibiotics, or anti-inflammatory drugs.

Probiotics. Probiotics are live microorganisms that can help restore the balance of good and bad bacteria in your gut. They may improve digestion, immunity, and reduce inflammation. However, not all probiotics are the same, and some may work better than others for different people with IBS.
Psychological therapies. Psychological therapies can help you cope with stress and emotional factors that may trigger or worsen your IBS symptoms. They can also teach you relaxation techniques and cognitive-behavioural strategies to change your thoughts and behaviours that may affect your gut-brain axis.
Alternative therapies. Alternative therapies are non-conventional methods that may help some people with IBS find relief from their symptoms. These include acupuncture, herbal remedies, massage therapy, aromatherapy, yoga, meditation, or tai chi. However, the evidence for the effectiveness and safety of these therapies is limited or conflicting, so you should be cautious and consult your doctor before trying them .
Conclusion:
Remember that IBS is a chronic condition that may fluctuate over time and require ongoing management. You may need to work with your GI doctor and other health professionals to find the best treatment plan for you .
Acknowledgment
About the author

Dr Nikhil Nanjappa M.S., FRCS Ed., M.IPD Ed.,M. FST Ed., has recently returned from the United Kingdom after serving as a Consultant Surgeon at St. James’s University Hospital, Leeds. He is a consultant surgical gastroenterologist and a colorectal surgeon. He is amongst only a handful of surgeons in the country with 3 years of super speciality training experience in colorectal surgery. He has extensive experience and is trained in advanced minimally invasive techniques for the management of Inflammatory bowel disease.