Fissure: Pain in the a$$
As a specialist colorectal surgeon, my primary goal is to provide you with accurate and easily understandable information about various conditions that can affect your digestive health. One such condition that often causes discomfort and concern is a fissure in ano. In this guide, we’ll delve into what a fissure in ano is, its causes, symptoms, types, diagnosis, and available treatments.
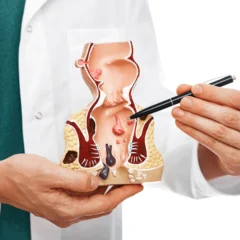
What is a Fissure in Ano?
A fissure in ano, commonly referred to as an anal fissure, is a small tear or cut in the lining of the anal canal. It’s a relatively common condition that can result in pain, discomfort, and sometimes even bleeding during bowel movements
Causes
The most common causes of anal fissures include:
1. Constipation: Straining during bowel movements due to hard stools can put pressure on the anal canal, leading to the development of fissures.
2. Diarrhoea: Frequent or prolonged episodes of diarrhea can irritate the anal area and increase the risk of fissure formation.
3. Trauma: Certain activities like passing large or hard stools, anal intercourse, or the insertion of foreign objects can cause trauma to the anal area, potentially leading to fissures.
4. Low-Fibre Diet: A lack of dietary fibre can result in hard stools, making it difficult to pass them without straining.
5. Spasm of Anal Sphincter: An involuntary tightening of the anal sphincter muscles can reduce blood flow to the anal area, impairing healing and causing fissures.
Symptoms
The symptoms of an anal fissure can vary but often include:
1. Pain: A sharp, burning pain during and after bowel movements is a common symptom. This pain can last for some time after you’ve finished using the toilet.
2. Bleeding: You may notice bright red blood on toilet paper or in the toilet bowl after a bowel movement. The bleeding is usually minimal but can cause anxiety.
3. Itching and Discomfort: The area around the anus may become itchy and uncomfortable due to the irritation caused by the fissure.
Types of Anal Fissures

There are two main types of anal fissures:
1. Acute Fissure: These fissures are relatively short-lived and often heal on their own within a few weeks with proper care and management.
2. Chronic Fissure: When a fissure persists for more than six weeks or becomes recurrent, it’s considered chronic. Chronic fissures may require more specialized treatment to promote healing.
Diagnosis
If you’re experiencing symptoms that suggest an anal fissure, it’s crucial to consult a medical professional, such as a surgical gastroenterologist or a colorectal surgeon. During your visit, the doctor will:
1. Take your Medical History: Understanding your medical history and any underlying conditions can help determine the cause of the fissure.
2. Perform a Physical Examination: A gentle examination of the anal area will help the doctor identify any visible fissures and assess their severity.
3. Digital Rectal Examination: A gloved, lubricated finger is inserted into the rectum to check for any abnormalities or tenderness. This may not be possible when there is severe sphincter spasm.
4. Anoscopy: A thin, flexible tube with a light and camera (anoscope) may be inserted into the anus to get a clearer view of the fissure and surrounding tissue. This may not be possible when there is severe sphincter spasm. This may not be possible when there is severe sphincter spasm.
Treatment
The treatment of anal fissures aims to relieve pain, promote healing, and prevent recurrence. Depending on the severity of the fissure, your doctor may recommend:
1. Lifestyle Changes: Increasing your fibre intake through a balanced diet and drinking plenty of water can soften stools, making bowel movements easier and less likely to cause trauma.
2. Topical Medications: Over-the-counter or prescription creams containing numbing agents, muscle relaxants, or nitroglycerin can help reduce pain and relax the anal sphincter muscles, aiding in healing.

3. Sitz Baths: Soaking your anal area in warm water for 10-15 minutes a few times a day can provide relief and promote blood flow to the area.
4. Botulinum Toxin Injection: In some cases, injecting botulinum toxin into the anal sphincter muscles can help relax them, reducing spasm and allowing the fissure to heal.
5. Surgical Intervention: If conservative methods don’t yield satisfactory results, surgical options like lateral internal sphincterotomy or advancement flap procedures might be considered. I barely ever suggest this, less than 2 patients a year.
Prevention

While some risk factors for anal fissures can’t be entirely avoided, adopting certain habits can help reduce the likelihood of developing them:
1. Maintain a Healthy Diet: A diet rich in fiber helps regulate bowel movements, preventing constipation and the associated strain.
2. Stay Hydrated: Drinking enough water keeps stools soft and easy to pass.
3. Practice Good Anal Hygiene: Gently clean the anal area after bowel movements and avoid excessive wiping, which can cause irritation.
4. Avoid Straining: If you’re having difficulty passing stools, don’t force it. Straining can worsen fissures.
5. Treat Underlying Conditions: If you have conditions like Crohn’s disease or inflammatory bowel disease, managing them effectively can reduce your risk of developing anal fissures.
Conclusion
Fissure in ano is a common and treatable condition that can cause discomfort but can be managed effectively with medical intervention and lifestyle adjustments. If you suspect you have an anal fissure, don’t hesitate to seek professional medical advice to ensure proper diagnosis and appropriate treatment.
Remember, your colorectal health matters, and taking proactive steps can lead to improved well-being and quality of life.
*Disclaimer: This article is intended for informational purposes only and should not be considered a substitute for professional medical advice. Always consult with a qualified healthcare provider for accurate diagnosis and appropriate treatment.*
Acknowledgement
Author

Dr Nikhil Nanjappa M.S., FRCS Ed., M.IPD Ed., M. FST Ed., has recently returned from the United Kingdom after serving as a Consultant Surgeon at St. James’s University Hospital, Leeds. He is a consultant surgical gastroenterologist and a colorectal surgeon. He is amongst only a handful of surgeons in the country with 3 years of super speciality training experience in colorectal surgery. He has extensive experience and is trained in advanced minimally invasive techniques for the management of haemorrhoids, fissures and fistulas.
For appointments visit www.drnikhilnanjappa.com or call +91081 27867