Inflammatory Bowel Disease(IBD): Once a rarity on our shores, now a reality!
What is inflammatory bowel disease?
Inflammatory bowel disease (IBD) is a term that refers to a group of chronic inflammatory conditions that affect the digestive tract. The two main types of IBD are ulcerative colitis and Crohn’s disease1. Ulcerative colitis causes inflammation and ulcers in the inner lining of the colon and rectum, while Crohn’s disease can affect any part of the digestive tract from the mouth to the anus, causing inflammation and damage to the deeper layers of the intestinal wall. What causes inflammatory bowel disease? The exact cause of IBD is not known, but it is believed to be a result of a complex interaction between genetic, environmental, immune, and microbial factors2. Some of the possible risk factors for developing IBD include:
Family history: People who have a close relative with IBD are more likely to develop the condition themselves.
Ethnicity: IBD is more common in people of European or Jewish descent, but it can affect anyone.
Age: IBD can occur at any age, but it usually begins before the age of 35.
Diet: Some studies have suggested that a Westernized diet, high in fat, sugar, and processed foods, may increase the risk of IBD.
Smoking: Smoking can worsen the symptoms and complications of IBD, especially Crohn’s disease.
Infections: Some bacterial or viral infections may trigger or exacerbate IBD in some people.
Medications: Certain drugs, such as nonsteroidal anti-inflammatory drugs (NSAIDs), antibiotics, oral contraceptives, and isotretinoin, may increase the risk or severity of IBD in some people.

How common is inflammatory bowel disease in India?
IBD is becoming increasingly prevalent in developing countries, including India. According to some estimates, India has about 1.5 million patients with IBD, second only to the USA with 1.6 million patients4. The incidence and prevalence of IBD in India are rising steadily due to changes in the diet and lifestyle, urbanization, industrialization, and exposure to environmental pollutants. However, there is still a lack of awareness and access to diagnosis and treatment for many patients with IBD in India. What are the symptoms of inflammatory bowel disease? The symptoms of IBD vary depending on the type, location, and severity of the inflammation. Some of the common symptoms include:
Diarrhea: Frequent and loose stools, sometimes with blood or mucus.
Abdominal pain: Cramping or discomfort in the lower abdomen.
Weight loss: Unintentional loss of appetite or malabsorption of nutrients.
Fever: Elevated body temperature due to infection or inflammation.
Fatigue: Feeling tired or weak due to anemia or dehydration.
Anemia: Low levels of red blood cells due to bleeding or inflammation.
Joint pain: Swelling or stiffness in the joints due to inflammation or arthritis.
Skin problems: Rashes, ulcers, or nodules on the skin due to inflammation or immune reactions.
Eye problems: Redness, pain, or blurred vision due to inflammation or uveitis.
Mouth sores: Ulcers or canker sores in the mouth due to inflammation or aphthous stomatitis.
How is inflammatory bowel disease diagnosed?
The diagnosis of IBD is based on a combination of medical history, physical examination, laboratory tests, imaging tests, and endoscopic procedures. Some of the tests that may be used to diagnose IBD include:

Blood tests: To check for signs of inflammation, infection, anemia, or nutritional deficiencies1.
Stool tests: To look for blood, mucus, parasites, bacteria, or markers of inflammation in the stool.
X-rays: To visualize the structure and function of the digestive tract and rule out other causes of abdominal pain or obstruction.
Ultrasound: To examine the organs and tissues in the abdomen using sound waves.
CT scan: To obtain detailed images of the cross-sections of the abdomen using X-rays and a computer.
MRI scan: To obtain detailed images of the soft tissues and organs in the abdomen using magnetic fields and radio waves.
Colonoscopy: To examine the inner lining of the colon and rectum using a flexible tube with a camera and a light source.
Sigmoidoscopy: To examine the lower part of the colon and rectum using a shorter version of a colonoscope.
Upper endoscopy: To examine the esophagus, stomach, and duodenum using a similar device as a colonoscope.
Capsule endoscopy: To examine the small intestine using a small capsule that contains a camera and a transmitter.
Biopsy: To take a small sample of tissue from the affected area and examine it under a microscope for signs of inflammation or damage.
How is inflammatory bowel disease treated?
The treatment of IBD aims to reduce the inflammation, control the symptoms, prevent or heal the complications, and improve the quality of life of the patients. The treatment options depend on the type, location, and severity of the disease, as well as the patient’s preferences and response to therapy. Some of the treatment options include:

Medications: Drugs that can help reduce the inflammation, suppress the immune system, relieve the pain, stop the bleeding, prevent or treat infections, or correct nutritional deficiencies. Some of the common medications used for IBD include:
Aminosalicylates: Anti-inflammatory drugs that are effective for mild to moderate ulcerative colitis and may also help some patients with Crohn’s disease.
Corticosteroids: Powerful anti-inflammatory drugs that are used for short-term treatment of moderate to severe IBD flare-ups.
Immunomodulators: Drugs that modify the immune system and reduce its overactivity in IBD.
Biologics: Drugs that target specific molecules involved in the inflammatory process in IBD.
Antibiotics: Drugs that kill or inhibit the growth of bacteria that may cause or worsen IBD.
Probiotics: Live microorganisms that may help restore the balance of the gut flora and improve the intestinal barrier function in IBD.
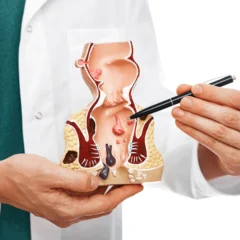
Surgery: A procedure that involves removing part or all of the affected intestine or creating an artificial opening for waste elimination. Surgery may be necessary for patients with severe or complicated IBD that does not respond to medications or causes serious complications such as perforation, obstruction, bleeding, fistula, abscess, or cancer1. Some of the common surgical procedures for IBD include:
Colectomy: Removal of part or all of the colon.
Proctocolectomy: Removal of the entire colon and rectum.
Ileostomy: Creation of an opening in the abdomen where the end of the small intestine is brought out and attached to a bag that collects the stool.
J-pouch: Creation of a pouch from the end of the small intestine that is connected to the anus and acts as a reservoir for stool.
Strictureplasty: Widening of a narrowed segment of the intestine without removing it.
Resection: Removal of a diseased segment of the intestine and rejoining of the healthy ends.
Diet and lifestyle: Changes in the diet and lifestyle that can help manage the symptoms, prevent or reduce flare-ups, and improve overall health and well-being in patients with IBD. Some of these changes include:
Eating a balanced diet that provides adequate calories, protein, vitamins, minerals, and fluids.
Avoiding foods that may trigger or worsen symptoms such as spicy, fatty, fried, or high-fiber foods, dairy products, alcohol, caffeine, or artificial sweeteners.
Taking nutritional supplements if recommended by the doctor to correct any deficiencies or malabsorption problems.
Drinking plenty of water to prevent dehydration and electrolyte imbalance due to diarrhea or vomiting.
Quitting smoking to reduce the risk and severity of IBD, especially Crohn’s disease.
Managing stress to lower its impact on the immune system and inflammation in IBD.
Exercising regularly to improve blood circulation, muscle strength, bone health, mood, and quality of life in IBD.
Conclusion
IBD is a chronic inflammatory condition that affects the digestive tract. It can cause various symptoms such as diarrhea, abdominal pain, weight loss, fever, fatigue, anemia, joint pain, skin problems, eye problems, and mouth sores. It can also lead to serious complications such as perforation, obstruction, bleeding, fistula, abscess, or cancer. The diagnosis of IBD is based on medical history, physical examination, laboratory tests, imaging tests, and endoscopic procedures. The treatment of IBD aims to reduce inflammation, control symptoms, prevent or heal complications, and improve quality of life.
Acknowledgement
About the author

Dr Nikhil Nanjappa M.S., FRCS Ed., M.IPD Ed.,M. FST Ed., has recently returned from the United Kingdom after serving as a Consultant Surgeon at St. James’s University Hospital, Leeds. He is a consultant surgical gastroenterologist and a colorectal surgeon. He is amongst only a handful of surgeons inthe country with 3 years of super speciality training experience in colorectal & IBD surgery. He has extensive experience and is trained in advanced minimally invasive techniques for the management of Inflammatory bowel disease.
For appointments visitwww.drnikhilnanjappa.com or call+91081 27867