Pouches in Your Colon: What You Need to Know About Diverticular Disease
What is it?

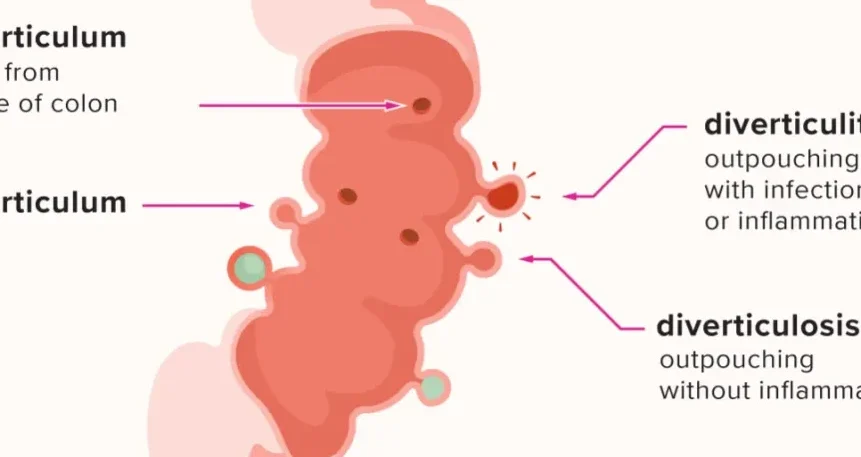
Diverticular disease of the colon is not an uncommon condition that affects the large intestine, or colon. The colon is the part of the digestive system that absorbs water and nutrients from food and forms stool. Diverticular disease occurs when small pouches, called diverticula, develop in the wall of the colon. These pouches can become inflamed or infected, causing pain and other problems.
Types
There are two main types of diverticular disease: diverticulosis and diverticulitis. Diverticulosis is the presence of diverticula in the colon without any symptoms or complications. Most people with diverticulosis do not even know they have it. Diverticulitis is the inflammation or infection of one or more diverticula, which can cause severe abdominal pain, fever, nausea, vomiting, constipation or diarrhea.

What causes it?
The exact causes of diverticular disease are not known, but several factors may increase the risk of developing it. These include:
Aging. The incidence of diverticular disease increases with age, especially after 40.
Obesity. Being seriously overweight increases the odds of developing diverticular disease.
Smoking. People who smoke cigarettes are more likely than nonsmokers to experience diverticular disease.
Lack of exercise. Physical activity helps promote normal bowel function and reduces pressure inside the colon.
Diet high in animal fat and low in fiber. A low-fiber diet makes the stool hard and difficult to pass, which can increase the pressure in the colon and cause diverticula to form. A high intake of animal fat may also contribute to inflammation and infection of the diverticula.
What are the symptoms?

The symptoms of diverticular disease depend on whether it is diverticulosis or diverticulitis. Diverticulosis usually does not cause any symptoms, but some people may experience mild cramps, bloating or constipation. Diverticulitis can cause sudden and severe pain in the lower left side of the abdomen, which may be constant or come and go. Other symptoms may include:
Fever and chills
Nausea and vomiting
Loss of appetite
Bleeding from the rectum
Change in bowel habits
What are the potential complications?
Diverticular disease can lead to serious complications if left untreated. These include:

Abscess. An abscess is a collection of pus that forms inside or around a diverticulum, which can cause infection to spread to other parts of the abdomen.
Perforation. A perforation is a hole or tear in the wall of the colon, which can allow stool and bacteria to leak into the abdominal cavity and cause a life-threatening condition called peritonitis.
Fistula. A fistula is an abnormal connection between two organs or tissues, such as the colon and the bladder, which can cause urine to leak into the colon or stool to leak into the bladder.
Stricture. A stricture is a narrowing or blockage of a part of the colon, which can cause difficulty passing stool and increase the risk of bowel obstruction.
How is it diagnosed?
The diagnosis of diverticular disease is based on the medical history, physical examination and various tests. These tests may include:
Blood tests. Blood tests can check for signs of infection or inflammation, such as elevated white blood cell count or C-reactive protein level.
Urine tests. Urine tests can check for signs of urinary tract infection or fistula, such as blood or bacteria in the urine.
Stool tests. Stool tests can check for signs of bleeding or infection in the colon, such as blood or pus in the stool.
Abdominal X-ray. An abdominal X-ray can show signs of perforation or obstruction in the colon, such as air or fluid in the abdominal cavity.
Abdominal ultrasound. An abdominal ultrasound can show signs of abscess or fistula in the colon, such as fluid-filled sacs or abnormal connections between organs.
Abdominal CT scan. An abdominal CT scan can provide detailed images of the colon and other organs in the abdomen, and show signs of diverticulitis, abscess, perforation, fistula or stricture.
Colonoscopy. A colonoscopy is a procedure that uses a flexible tube with a camera and light to examine the inside of the colon and rectum, and show signs of diverticulosis, diverticulitis or bleeding. Timing of the colonoscopy is vital, if done too early may result with catastrophic complications.
How is it treated?

The treatment of diverticular disease depends on the type and severity of the condition. The main goals are to relieve symptoms, prevent complications and avoid recurrence. The treatment options may include:
Diet changes. For mild cases of diverticulosis or diverticulitis, eating a low residue diet during the acute flare and switching high-fiber diet after can help soften stool and reduce pressure in the colon. Drinking plenty of fluids can also help prevent dehydration and constipation. Avoiding foods that may irritate or get stuck in the diverticula, such as nuts, seeds, popcorn or corn, may also help prevent inflammation and infection.
Medications. For mild to moderate cases of diverticulitis, antibiotics can help treat infection and inflammation. Pain relievers, antispasmodics, can help.
Hospitalisation. For severe cases of diverticulitis, hospitalization may be needed to receive intravenous fluids and antibiotics, and to monitor for signs of complications. In some cases, surgery may be required to drain an abscess, repair a perforation, remove a fistula or stricture, or remove part of the colon.
Surgery. Surgery is usually reserved for people who have recurrent or complicated diverticulitis, or who do not respond to medical treatment. The most common type of surgery is called a bowel resection, which involves removing the diseased part of the colon and reconnecting the healthy ends. Sometimes, a temporary or permanent colostomy may be needed, which involves creating an opening in the abdomen for stool to pass out of the body into a bag.
Conclusion
Diverticular disease of the colon is not uncommon and often asymptomatic condition that can cause serious problems if complications develop. By following a healthy lifestyle and seeking medical attention with specialist colorectal surgeons, most people with diverticular disease can prevent or manage their condition and enjoy a good quality of life.
References
1: Diverticulitis – Symptoms and causes – Mayo Clinic 2: Diverticular disease of the colon – Harvard Health 3: Diverticulosis and diverticulitis – Better Health Channel
Author

Dr Nikhil Nanjappa M.S., FRCS Ed., M.IPD Ed.,M. FST Ed., has recently returned from the United Kingdom after serving as a Consultant Surgeon at St. James’s University Hospital, Leeds. He is a consultant surgical gastroenterologist and a colorectal surgeon. He is amongst only a handful of surgeons in the country with 3 years of super speciality training experience in colorectal surgery. He has extensive experience and is trained in advanced minimally invasive techniques for the management of haemorrhoids, fissures and fistulas.